Pediatric Hematology & Oncology Fellowship
Johns Hopkins University/National Institutes of Health Pediatric Hematology-Oncology Fellowship
The Johns Hopkins University School of Medicine and the National Cancer Institute represent two of the of the most distinguished pediatric hematology-oncology centers in the world, and their joint fellowship provides exceptional training to six new fellows per year. The program’s mission is to train diversely talented clinician-researchers who will become leaders in the field of pediatric hematology-oncology.
The program is led by
 Stacy Cooper, MD, Program Director
Stacy Cooper, MD, Program Director
 Emily Rao, MA MD, Associate Program Director
Emily Rao, MA MD, Associate Program DirectorMeet Our Faculty and Alumni
Our Faculty
The Johns Hopkins University/National Institutes of Health fellowship in pediatric hematology-oncology is able to capitalize on three distinct Divisions, each with complementary expertise in both clinical and research venues:
Johns Hopkins University Division of Pediatric Hematology
Johns Hopkins University Division of Pediatric Oncology
National Institutes of Health Pediatric Oncology Branch
Our Faculty with Research Focus
View faculty with research focus
Our Alumni
View current positions of former trainees
Fundamental Program Facets
- Comprehensive clinical training at both Johns Hopkins Children’s Center and the National Cancer Institute
- Optimal clinical education achieved by active patient care in a fellow-centric model
- Highly protected research time to allow for productive scholarship during years 2 and 3, with an optional guaranteed fully funded fourth year of research
- World renowned experts who are committed to mentorship
- Active promotion of fellow wellness
- Individualization of training to capitalize on each trainee’s full potential
Unique Aspects and Opportunities
- Diverse patient population with a wide array of disease pathology ranging from common to rare diseases allow for well-rounded clinical training.
- Opportunity to care for many active clinical trial patients receiving cutting edge therapies both at Johns Hopkins Children’s Center and the NIH.
- Train at one of only a handful of hospitals in the US that operates a robust international medicine program bringing complex patients from around the world, paired with an in-house care coordinator/translator who accompanies patients to their visits.
- Training at the only Hemophilia Treatment Center in the state.
- Exposure to patients with rare diagnoses through NIH programs.
- Specialty training programs
- Guaranteed option of a fourth year of protected research
- Fully funded PhD opportunity through the Cellular and Molecular Medicine program
- Dual-board training in adult and pediatric hematology-oncology
- Dual-board training in pediatric hematology-oncology and palliative care
- Focus on educational innovation in fellowship training
- Strong track record of successful grant funding during fellowship to launch fellows into robust research careers after training
- The Baltimore/Bethesda area has so much to offer including elegant architecture, exciting food scene, Baltimore Orioles & Ravens games, state parks, and train access to other points of interest with a lower cost of living than most other east coast cities.
Program Curriculum
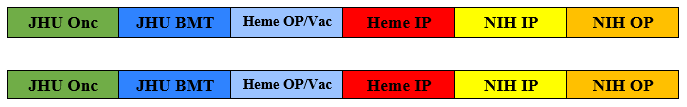
The first year of fellowship is composed of 11 months of clinical training and 1 month of vacation. Fellows will rotate through the following 1 month blocks twice in the first year of training:
Our fellowship leadership has worked hard to provide extremely protected time in the 2nd and 3rd years of fellowship to allow for development of rigorous fellow research projects. Clinical requirements in 2nd and 3rd years consist solely of ½ day per week of continuity clinic and 4-5 weekends on inpatient hematology.
Fellows have the option to stay on for an optional fourth year of advanced training, which allows for additional dedicated research time as well as the option of focused clinical training, with formal 4th year training programs in non-malignant hematology, neuro-oncology, sarcoma, bone marrow transplant, and cellular therapy.
Want to learn more about what our fellows are up to? Follow them on Instagram @hopkins_nih_pho_fellowship
How to Apply
Candidates should apply through the Electronic Residency Application Service (ERAS), and are matched through the National Residency Matching Program (NRMP). Interviews begin in September, and will be virtual via Zoom for the 2021 season. A holistic review of the application is conducted for each candidate who applies.
Who to Contact
For additional information or any questions, please email [email protected] or contact Gladys Valencia Novak, program administrator, at 410-614-5055.

