Deep Vein Thrombosis (DVT) / Thrombophlebitis
The term venous thromboembolism (VTE) is used to describe two conditions, deep vein thrombosis (DVT) and pulmonary embolism (PE). This term is used because the two conditions are very closely related. And, because their prevention and treatment are also closely related.
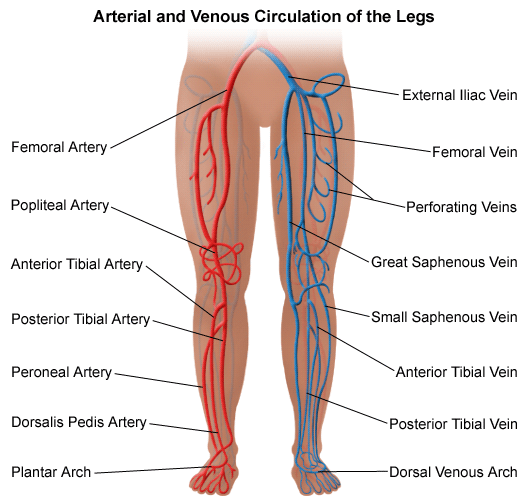
Deep vein thrombosis is a blood clot or thrombus in a deep vein. They are most common in the leg. But they may develop in the arm or other part of the body. Part of the clot, called an embolus, can break off and travel to the lungs. This is a pulmonary embolus (PE). This can cut off the flow of blood to all or part of the lung. PE is an emergency and may cause death. If you have symptoms that may indicate a blood clot in the lungs, call 911 or get emergency help. Symptoms of a blood clot in the lungs include chest pain, trouble breathing, coughing (may cough up blood), a fast heartbeat, sweating, and fainting.
Two other complications of a blood clot are chronic venous insufficiency and post-thrombotic syndrome.
-
Chronic venous insufficiency may happen following a blood clot in a leg vein. It means that a vein no longer works well. It is a long-term condition where blood pools in the vein instead of flowing back to the heart. Pain and swelling in the leg are common symptoms.
-
Post-thrombotic syndrome may also happen following a blood clot in a leg vein. It is a long-term problem with pain, swelling, and redness. Ulcers and sores can also happen. All of these symptoms may make it difficult to walk and take part in daily activities.
What are the risk factors for deep vein thrombosis?
Risk factors include:
-
Overweight or obesity
-
Blood clotting disorder
-
Age over 60 years
-
Surgery
-
A long period of not moving, for example, when in the hospital or on a long trip
-
Birth control pills or hormone replacement therapy
-
Certain diseases and conditions, such as:
-
Previous blood clot
-
Varicose veins
-
Heart problems, such as heart failure, or heart attack
-
Inflammatory bowel disease
-
Lupus, a disease of the immune system
-
Cancer and some cancer treatments
-
-
Paralysis
-
Pregnancy
-
Having a central venous catheter, for example, in a large vein in the chest
What are the symptoms of deep vein thrombosis?
Deep vein thrombosis may happen without symptoms. Common symptoms include pain, swelling, and redness in the leg, arm, or other area.
These symptoms may mean that you have a blood clot. The symptoms of a blood clot may also look like other medical conditions. Always see your healthcare provider for a diagnosis.
How is deep vein thrombosis diagnosed?
Along with a medical history and physical exam, your healthcare provider may do other tests including:
-
Duplex ultrasound. This procedure involves placing ultrasound gel on the affected area and then moving a handheld device across it. A picture of the blood flow is displayed on a monitor. Duplex ultrasound is the most common test for DVT.
-
Lab work. Blood work may be done to look for blood clotting and other problems.
What is the treatment for deep vein thrombosis?
Specific treatment will be determined by your healthcare provider based on:
-
How old you are
-
Your overall health and medical history
-
How sick you are
-
The location of the clot
-
How well you can handle specific medicines, procedures, or therapies
-
How long the condition is expected to last
-
Your opinion or preference
The goal of treatment is to prevent the clot from getting larger, to prevent a blood clot from traveling to the lungs, and to decrease the chance of another blood clot forming.
Treatment may include:
-
Blood thinners (anticoagulant medicines). These medicines decrease the ability of the blood to clot. Examples of anticoagulants include warfarin and heparin. Other anticoagulants may also be used, including rivaroxaban, apixaban, dabigatran and enoxaparin. The most common side effect of blood-thinning medicine is bleeding. Report bruising or bleeding to your healthcare provider right away. You may have blood in the urine, bleeding with bowel movements, a bloody nose, bleeding gums, a cut that will not stop bleeding, or vaginal bleeding.
-
Clot busters (fibrinolytics or thrombolytics). These medicines are used to break up clots.
-
Inferior vena cava filter. In some cases, a filter is placed in the vena cava (the large vein which returns blood from the body to the heart). This filter prevents clots from reaching the heart and lungs.
How can deep vein thrombosis be prevented?
Preventing deep vein thrombosis can include:
-
Anticoagulant medicines are given to certain patients having surgery to prevent blood clots.
-
Wiggling the toes and moving the ankles helps to prevent blood clots caused by long periods of sitting or lying down.
-
When you travel and must sit for long periods of time, you can reduce your risk of a blood clot by doing the following:
-
Walk up and down the aisles (if traveling by plane or bus)
-
Stop about every hour and walk a little (if traveling by car)
-
While sitting, move your legs, ankles, and toes
-
Wear loose clothing
-
Limit the amount of alcohol you drink
-
Drink a lot of water and other healthy drinks
-
Prevention may also include:
-
Walking. Getting up and moving as soon as possible after surgery or illness
-
Sequential compression device (SCD) or intermittent pneumatic compression (IPC). Special sleeves go around both legs. They are attached to a device that applies gentle pressure to the legs. Remove the sleeves so that you do not trip or fall when you are walking, such as when you use the bathroom or shower. Ask for help if you cannot remove and replace the sleeves.
-
Elastic or compression stockings, if prescribed by your healthcare provider.





