Beyond Memory Loss: How to Handle the Other Symptoms of Alzheimer's
There is a lot of talk about the emotional pain patients and caregivers suffer when a loved one loses memories to Alzheimer’s. But what about the other symptoms? Here are tips from a Johns Hopkins expert on what to watch for and how to manage.

Alzheimer’s is known as a disease of lost memories. But what many of us may not understand—until faced with it in our own loved ones—is that memory loss is just the beginning. Depression, anxiety and agitation, and sleep-related problems also plague people with Alzheimer’s disease.
Left untreated—as they too often are—these symptoms can have a significant effect on quality of life and even on the course of the disease itself. Recognizing and treating these behavioral and cognitive symptoms, on the other hand, can go a long way toward improving the quality of life of both caregivers and patients, and may even help with some of the cognitive symptoms, if only for a short time.
Johns Hopkins expert Andrea Nelson, R.N., highlights several of the most common non-memory-related symptoms, along with treatments that offer hope for relief.
Depression
Between 40 and 50 percent of people with Alzheimer’s experience depression, Nelson says, compared with about 7 percent of the general population. The high incidence is related both to changes in the brain from the disease and, at least early in the disease, the shock of diagnosis.
Johns Hopkins has been on the forefront of recognizing depression in people with Alzheimer’s disease, with Johns Hopkins psychiatrists coining the term “affective syndrome of Alzheimer’s disease” more than a decade ago to describe the depression that occurs in these patients.
People with Alzheimer’s who are depressed tend to be apathetic and irritable and to have sleep disturbances, but they are less likely to feel guilty or have a risk of suicide than depressed people without Alzheimer’s.
Treatment
“A lot of times if you treat the depression, people’s quality of life really improves,” Nelson says. “You may even see a few upticks in their memory.” Treatment for depression typically involves the use of medications called selective serotonin reuptake inhibitors (SSRIs), which may also help with anxiety and agitation.
Anxiety and Agitation
These conditions can manifest as emotional distress, excessive movement, aggression, disruptive irritability, and loss of inhibition. The anxiety and agitation are more apparent in the early stages of the disease as people begin to recognize their losses and the seriousness of the disease, Nelson says. Later, they may become anxious about being left alone or abandoned, while any changes in the daily routine can also trigger anxiety and agitation.
Treatment
The most common treatment for anxiety and agitation is low doses of atypical antipsychotic medications such as risperidone and olanzapine. However, the drugs may increase the risk of strokes, heart attacks and death in older people. Meanwhile, anti-anxiety drugs such as diazepam can lead to dizziness and falls in older people.
Antidepressants can often help. A clinical trial at Johns Hopkins evaluating the use of the antidepressant citalopram in people with Alzheimer’s and anxiety found that it was safer and at least as effective as currently used antipsychotic drugs.
Sleep Disruptions
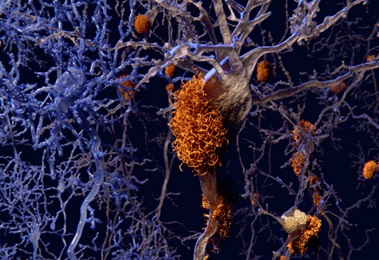
Studies find that people with Alzheimer’s disease spend more time awake than those without. In fact, changes in sleep pattern may be an early sign of the disease, with one study finding that the brains of older adults with poor sleeping habits were more likely to have amyloid plaque deposits, the sticky protein fibers that are a hallmark of Alzheimer’s disease. Researchers speculate that treating sleep problems early could minimize this effect and, potentially, prevent or slow the progression of the disease, although that is still speculative.
Treatment
The most important treatment for sleep disruptions is not sleeping pills, but activity, says Nelson. “If they’re up at night and sleeping during the day, we recommend activities. Walking, an adult day center, anything to get them more active during the day so they sleep better at night,” she says.
Treatment Memory Care Services from the Comfort of Home